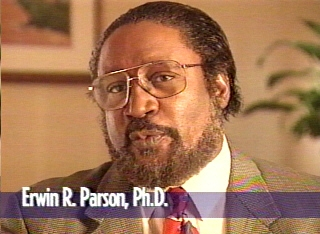
© Erwin Randolph Parson, Ph.D., A.B.P.P.
INTRODUCTION
| When disasters strike they are sudden, unexpected, and “earth-shattering” to those affected by them. Often those who are exposed directly talk about how their lives of relative tranquility before the disaster has been radically changed, and how peace of mind has evaporated and replaced by worry and catastrophic expectations. They describe their new post-disaster reality as living life “upside down,” in a state of confusion, and pervasive anxiety, and helplessness. Disasters are generally defined as mass environmental stress affecting a large number of people. Terrorism, like no other mass disaster event, smashes to smithereens a victim’s sense of normality and reality, while eroding the sense of safety and general well-being.Disaster victims also speak about things not being the same, of how their inner sense of safety and the ability to count on the stability of the environment (for even a modicum of predictability) has been lost. Some also speak about feeling powerless, having lost the structure of their daily lives and associated routines, and about the collective emotional distress caused by the abrupt depletion of resources and altered physical environments.The contents of this article is based on: (1) the author’s over two decades of clinical, consultative, scientific, instructional, and administrative expertise in the area of traumatic stress, (2) the author’s direct professional activities with victims of disasters, to include the September 11th attack by terrorists on the World Trade Center in New York City during seven trips to the City beginning October 10, 2001, and (3) knowledge gleaned from decades of clinical and field studies on specific disasters in the United States and in many countries of the world. Specifically, the author has participated in helping victims exposed to the Loma Prieta Earthquake of 1989 in northern California, the Perryville Explosion of 1991 in Perryville, Maryland, the Oklahoma City Bombing of 1995, the Polish Flood of 1996, Hurricane Floyd of 1999, and the World Trade Center (WTC) attack of September 11, 2001.THE REALITY AND INCIDENCE OF DISASTERSDisasters are found everywhere in the United States and around the world, and can be traced throughout the history of human existence. Historically, we find various parts of the world had endured tidal waves, famines, earthquakes, floods, mining accidents, bombings, industro-chemical explosions, bush fires, mudslides, and pestilence, to include the Great Plague of Europe between 1347 and 1350.Though most victims interviewed in New York City by this writer showed symptoms of Acute Stress Disorder or Post-Traumatic Stress Disorder, responses were diverse. This diversity of stress response can be expected given the differing personality styles, prior experiences, prior traumas, and the general mental health of these individuals prior to the flood, typhoon, earthquake, or industrial accident.Disaster stress research studies have revealed that these untoward events affect the lives of people for years and even decades. Understanding the effects of these disaster events upon victims’ minds, bodies, relationships, and behavior, is crucial for survivors and therapists. This understanding may serve preventive ends in guarding the individual against traumatic symptoms that may potentially undermine personal, social, and occupational (economic) functioning.Diversity of Disaster Traumatic IncidentsIn Brende’s (1998) article, “Coping with Floods: Assessment, Intervention, and Recovery Processes for Survivors and Helper,” he discusses “unprecedented and destructive flooding in various parts of the United States … particularly during 1997 and 1998” (p. 107). He notes that flooding represents about 40% of all natural disasters.There are a wide variety of natural disasters-tornadoes, floods, hailstorms, hurricanes, droughts, heat wave, Western fires, tropical storms, ice storms, and earthquakes. Disasters are very costly to victims-in terms of money, life disruption, loss of resources, loss of a sense of community, loss of property, and becoming homeless for a protracted period of time. Two noteworthy examples of high cost disasters in the United States both in 1989 were the Loma Prieta Earthquake, and Hurricane Hugo. According to the United States National Committee for the Decade of National Disaster Reduction, thousands were homeless for over a year, while the economic cost exceeded $15 billion.Technological accidents are examples of human-caused disasters. These are disasters characterized the unintentional action (or inaction) of an individual, group, or organization resulted in an overwhelming environmental situation that resulted in mental, physical, and economic harm to people. Technological disasters are human-caused events, but are not by design. Examples of this class of disasters are the 1986 Chernobyl nuclear accident in the Soviet Union, the 1984 gas leak in Bhopal, India, and the 1979 Three Mile Island of nuclear leak in Harrisburg, PA. and a number of serious mining accidents, and devastating explosions due to bombings over the years. Scientists have found that, compared to human-engineered disasters, technological disasters are significantly less distressing, with lower prevalence rates of post-traumatic stress disorder (PTSD). This is also true for acute stress disorder (ASD) rates: industrial accidents produce a rate of 6%, compared to a 33% rate for mass violence (shooting)(Bryant, 2000; Bryant & Harvey, 1997).Terrorism-related and technological disasters inflict serious injuries, caused by flying debris, and intense thermal exposure. The victims of terrorism explosions often report varying degree of burns and blast injuries that produce hearing loss, serious internal injuries-to the intestines, to the head (to include closed head damage), abdominal contusions, facial and orbital lacerations, and injuries of pancreas, heart, lung, and parts of the central nervous system.The terrorism waged against the World Trade Center in 1993, and the hijacking of four planes on September 11, 2001 that resulted in the worst terroristic attack on the United States, are examples of human-engineered disasters. Clinicians and scientists believe that human-engineered disasters have a greater and more profound and enduring effect on the victim than natural disasters in which no human design existed (Parson, 1995a, 1995b).DISASTER TRAUMATIC STRESS RESPONSE (DTrS)Stress causes the body to release neurochemicals that can cause surges in blood pressure and heart rate. Heart attacks have increased after catastrophic situations and are well documented. When adults and children are exposed to disasters, they experience a constellation of stress responses or symptoms that are seen in victim/survivors across disaster types-natural, “human-caused” (or technological), and “human-engineered” (intentional) disasters. As outlined here, the Disaster Traumatic Stress Response consists of intense fears, anxiety, panic, increased arousal, re-experiencing of the trauma-in nightmares, flashbacks, and unbidden ideation; avoidance, numbing, anger, irritability, guilt, shame, grief, depression, distortions of self-experience (to include various forms of dissociative process), sexual dysfunctions, substance abuse, drug abuse, and feelings of panic and other anxiety disorders. As such DTrS encompasses Post-Traumatic Stress Disorder, but goes beyond it to include other trauma-based human responses not covered by the PTSD diagnosis. These “beyond” responses or components of DTrS involve social, political, economic, and ethnocultural factors.Biologically-Based SymptomsNeurophysiological Stress Response |
| Bodily tensionsFatigueNightmaresFlashbacksAnniversary reexperiencingJitteryBody injuries, aches, and painsExhaustion due to lack of sleepCardiovascular reactivity and “racing” heartGastrointestinal distressDisorder of sexual desire | Low back painEasily startledIrritabilityIncreased levels of cortical and norepinephrineInsomnia problemsHyperarousalElevated blood pressureMuscle crampsHeadachesChanges in appetiteRespiratory problems |
| Dissociation (feelings of being unreal, “blank” and “spacey”)Low self-esteem due to sense of failure and lack of self-efficacy.Loss of hope, faith, will, motivation, or purpose in one’s life.Feeling of profound emptiness.Sense of injustice.Feelings of being “in pieces” or fragmented, “scattered.”Difficulty making decisions.Internal sense of “breakdown” and chaos.Emotional numbing.Active expectation of future catastrophe (more terroristic attacks, more bioterrorism threats and dangers).Mental disorientation/disorganization.Impaired motivation.Feeling “overwhelmed” by unbidden memories and affects. | Basic absence of joy and pleasurePersistent search for security.Narcissistic injury and resentment toward the authorities.Self-blaming.Apathy.Reduced self-esteem.Counter-tender tendencyInner sense of disorganization.Feeling profoundly distant from corpus of societyDistrust.State of the self traumatic dreamingFeeling distant from others.Fear of intimacyLack or lowered sexual desire.Loss-based griefShame.Survivor guiltGuilt over what one did to remain alive.Self-responsibilitizing GuiltFeeling neglected and abandoned |
| Fear.Shock.Anxiety.Anger.Terror.Dramatic mood changes-ups/downsSadness.DepressionGrief. | Shame.Resentment over foreign intruders killing Americans and attempting to destroy the American way of life.Revenge motivation.PhobiasFear of flying on commercial airlines.Obsession with death, loss, fire, smoke and debris. |
| Mental confusionConcentration problemsMemory impairment.Denial.Repetitive vivid memories of trauma.Decrease in decision-making efficacy.Diversity of “triggering” mechanisms. | Amnesia-problems remembering aspects of the original traumatic event.Attention problemsUnbidden memoriesImpoverished attention span.Suspicion of Arabs and dark-skinned peopleExcessive worry. |
| Social isolation.Increased interpersonal conflict.Over-protectiveness toward spouse, children, friends, and other significant others.Distrust of others and reduced sense of community.Intimacy avoidanceStrained relationships and interpersonal conflicts. | Subway avoidance (reported particularly in WTC victims).Tall buildings avoidance (seen in WTC victims).Elevator avoidance (seen in WTC victims).”Ground Zero” area avoidance (WTC victims).Avoidance of Manhattan by people from the other four Boroughs (Brooklyn, Queens, Bronx, and Staten Island)Instrumental substance abuse. |
| Victim’s basic personality-the individual’s early and later developmental history.History of unsuccessful coping.Intensity of exposure.Exposure to extreme environmental devastation.Intensity of loss-relational, material (home, community, possessions, etc.), and economic losses. | Proximity to the epicenter of imploding building collapse (degree of exposure).Exposure of prior trauma (disasters, sexual abuse, motor vehicular accidents, etc.).Major life stressors.Physical illness/disability.Low socioeconomic status, poverty, and homelessness. |
| DV1. Victims who were injured or helplessly pinned down in a building and were rescued by first responder team members. DV2. Victims who were in a building and were rescued at a later time by firefighters, police, or emergency workers. Firefighters who entered the imploding buildings (and were able to escape) are also classified as DV2. | DV3. Victims who were actually in one of the WTC Towers and escaped from the building before it imploded, but witnessed impact of the collapse, and flying debris. DV4. Firefighters who experienced the implosion of the buildings. DV5. Firefighters who experienced the day-to-day exposure to being first to find and rescue missing persons in the rubble of fallen buildings. |
| Peripheral-Immediate Victims (PIVs)PV1. Persons in nearby buildings who witnessed a plane hit the first or second Tower, individuals living in the vicinity of the disastrous implosions who witnessed the fire, smoke, ashes, bent steel, and flying debris, as well as seeing people running to get away from the towering inferno. PV2. This subcategory includes emergency rescue workers, emergency medical workers, on-site crisis mental health providers, and media reporters. It is understood here that many PVs may actually be DVs: some emergency workers’ actual exposure to traumatizing stimuli may be at greater risk for traumatic symptoms and disorders.Relational Victims (RVs)RV1. Children who lost a parent in the disaster. RV2. Bereaved individuals with children whose spouse was killed in the disaster. RV2. Bereaved individuals whose spouse was killed in the disaster. RV3. Individuals whose friend or friends perished in the rubble. Vicarious Victims (VVs)Persons deeply affected by the deaths and destruction witnessed on television and other news stories and images of planes repeatedly hitting the WTC buildings. This classification of affected people can be found in New York, throughout the United States, as well as around the world.Stressors of First Responders-Firefighters, Police Officers, and Emergency WorkersFirst response personnel are at high risk for severe post-traumatic stress, and serious health problems. For example, first responder teams at the WTC were exposed to: |
| The experience of day-to-day exposure to an environment of ubiquitous destruction and death immersion.Exposure to mass violence.Chronic levels of fatigue.Exposure to bits and pieces of human remains, which may include parts of fellow FDNY and NYPD victims.Exposure to decaying, putrid human remains | Exposure to extreme environmental toxic, chemical substancesExposure to precipitate from tons of debris-particles in powder form consisting of ground glass, ground concrete, asbestos, and an incredible cocktail of multiple chemicals from computer chips, plastics, gas fumes, and radioactivity.Sudden-death-at-any-moment stress (as recovery workers do their work at “Ground Zero”). |
| Stress Reactions of First Response TeamsFirst response teams may experience the following traumatic stress responses: |
| Uncontrolled exposure due to passionate, intense desire to find/recover remains of fellow firefighters (“FDNY as Family-firefighters as brothers”).Self-imposed exposure.Identification stress (identification with dead fellow firefighters ).Feeling tainted by death.Incapacity to disengage from recovery efforts.Survivor guilt (“Why he and not me?”).Sensory reliving: “Smell of death.”Sensory reliving: “Sight of death.” | Sensory reliving: “Skin contact of death.”Sensory reliving: “Whole-body memories.”Chronic medical illnesses, especially respiratoryInability to grieve.Persistent sense of failure (due to unrealistic intention of finding and recovering all the injured and dead).Profound impacted grief.Experiencing the “death taint.”Resurgence of prior traumatic experiences. |
| Reassure, reassure, reassure! About safety, safety, safety! Focus on safety and offer credible reasons why they are truly safe (“I know you are safe because …”). Listen to them-hear and understand their reports, thoughts, and feelings, because what they have to say expresses important meaning for them. | As parent or teachers continually reassure and reiterate safety and security to the child, interweave their own concerns and fears with your explanations. Look for changes in the child’s behavior-in the home, school, in his or her relationship with peers, and degree of “comfort” with spending time alone-in isolation from others. |
| Impart basic trauma information (education about trauma dynamics, symptoms, and what is available in terms of interventions for themselves family members represent a first series of steps. Ensure that immediate psychological, medical, and material sources needs are met. Social support network. Techniques are clinical (with no apologies, as opposed to CISD’s non-Clinical). Features multiple sessions (compared to CISD’s single- session format). Sessions are short and manageable (45 minutes each sessions as opposed to CISD’s single session lasting three or four hours). | Initial screening. Initial assessment. Specific techniques to assuage hyperarousal. Specific techniques to manage stress. Specific techniques to manage catastrophic cognitive tendency through cognitive restructuring. Opportunities for individual and group sessions conducted in a noncoercive, democratic environment several days after the disaster (not in the first few days after the disaster). |
| Assessment is geared to determine the quality, intensity and course of acute stress reactions, as well as the victim’s coping efficacy. The approach is adaptable, and its application is based on the specific, screening and assessment-driven needs of the individual victim (as opposed to a one-size-fits-all approach). Unlike CISD, EPD offers intervention to direct victims, but only after several days have elapsed.Additionally, due to the specific problems posed by hyperarousal, dissociation, avoidance, and victims’ catastrophic cognitive tendency (tendency to catastrophize everything), EPD addresses these issues, and employs stress management procedures and cognitive restructuring that help manage hyperarousal and forestall hypersensitization and psychobiological decline in some direct victims. The tendency to dwell on calamitous thoughts that reinforce negative symptoms is a risk for severe distress and disorder in both the early and later phases of the post-disaster traumatic stress.The initial screening during Phases 1, 2, 3, or 4 can have varying degrees of efficacy in terms of forestalling the development of PTSD. Determining whether or not to conduct mental health screening and/or assessment is critical in the early phase of a disaster. The earlier the initial screening or initial assessment the better for the pretertraumatically stressed victim. Experience has shown that conducting initial data gathering sessions is important, but is not easy for a variety of reasons. First, logistical considerations may preclude these measures. Second, during the immediate phase victims are trying hard to get back to normal, and in doing so in the throes of perplexity, mystification, bewilderment, and normal denial and avoidance.Despite the need for more research in specific areas (e.g., timing of interventions, type of intervention and non-intervention, timing of initial screening, and initial assessment), some guidelines are nevertheless available at the present time. This writer, based on his clinical and field observations at “Ground Zero” and interventions and consultations with other disaster victims recommends that all victims classified above as DVs and PIVs should be screened (given the victim’s willingness and logistical flexibility) and receive early intervention. Other types of victims (e.g., VVs and RVs) may not require early screening or assessment until much later post-disaster.Due to early active avoidance and denial in disaster victims, which is widely known to be harmful in the long-run, the clinician is encouraged to be aware of what to say and how to say it to help victims overcome initial resistance. Here are some issues that need to be presented to victims in clear language to motivate them to get the help they need. This help often begins with initial screening and early assessment for DIVs and PIVs. Victims need to know that: |
| Disaster trauma, especially when human engineered, carries with it serious consequences and impairments-in sexual desire and functioning, Victims with a history of cardiovascular disease, major depression, substance abuse, and other mental disorders are at risk for severe forms of distress and dysfunctions. Trauma creates alterations in neurochemicals and immune systems that may lead to significant medical problems, and undermine the body’s recovery from illnesses. |
| In this writer’s experience in New York City post-911, many reluctant victims appeared to fear learning more about traumatic stress. Some seemed to believe that ignorance is bliss: that the less they knew the less the burdens and distress would be. These victims required specific educational materials to take home, read, and offer feedback to a therapist or designated individual or family members. They were encouraged to engage information-gathering sessions rather than therapy per se. Additionally, some found the concept of later treatment easier to accept with sensitive talk about the need to avoid the ills of traumatic stress, that therapy works, and that they need not consign themselves (DVs and PIVs) to a life of suffering alone.Post-Disaster Phases: From Acute Distress to Healing and IntegrationThe author’s experience and extant trauma and disaster clinical and research literature identify a number of phases people go through on the road to recovery (Brende, 1998; Brende & Parson, 1985; Parson, 1995a, 1995b, and Raphael, 2000) have identified five stages. Naturally, the time it takes for a particular victim to traverse these phases is expected to differ, depending on a number of variables-intensity of exposure, personality factors, resources availability, quality of social support networks, and the capacity to process fear, anxiety, and catastrophic cognitive processes. These phases, as conceptualized here, are meant to offer only a general point of reference (or benchmark) to portray the normal stress recovery process, and what can interfere with this process, and produce a mental disorder. Thus, the specific phase the victim is going through at the time may inform the particular intervention or non-intervention needed by a particular victim.This writer’s experience shows that disaster trauma victims use specific coping strategies based on the particular phase (or natural recovery configurations of symptoms being processed) at a given time after the trauma. It is recognized here that most people affected in the wake of disasters do not suffer PTSD in the immediate aftermath. A small percent of victims do reach criteria for PTSD in the immediate aftermath of a disaster. Many victims will experience evanescent stress responses that will abate over time. Though it is well known that a diversity of responses-based on individual differences, mental state and physical health status, prior trauma, etc.-can be expected among victims, it is also established that patterns of response may be based upon the natural processing of the trauma in the minds and bodies of those affected.Certainly, the role of denial is quite remarkable: some victims do not believe they need help from anyone-family, friends, nor professionals-to successfully recover from post-traumatic stress. Becoming stuck in this position is perhaps one of the most harmful places to be for DVs and PIVs. This belief may prove detrimental in that it may prevent distressed victims from seeking and benefiting from stress-ameliorating social networks and engaging in normal routines. Most people overcome the adverse effects of disasters, and go on to benefit and find positive outcomes.The proposed phases often overlap. They are: Emergency Adaptational Coping (EAC); First Stress Response Control (FRC); Reenactment and Mastery (RAM); Cynicism and Reflective-Transformation (CRT); and Trauma Resolution Vs. Stress Disorder (TRvsSD).Phase 1-Emergency Adaptational Coping (EAC)During this first phase of the disaster recovery process the victims experience their lives as being threatened and respond with fear, shock, disbelief, horror, helplessness, and an accompanying physiological “fight-flight” activation of pulse, blood pressure, respiration, heart rate, muscle activity, and release of such hormones as adrenaline. This phase begins immediately after the disaster.The September 11th attack on the World Trade Center was a shocking event that has profoundly affected Americans and the world. According to people who were inside the imploding Towers, and those in the vicinity of the disaster, and falling debris, smoke, and flying body parts, glass, and metal, the event was traumatically memorable, and emotionally painful. Shattering of the sense of self and reality accounts for the feeling of unreality, strangeness, and disorientation mentioned to me by many traumatically shocked victims. As is true of many other kinds of disasters, people worried about the quality of the air they were breathing in the City, many having heard of the potentially toxic cocktail of lead, asbestos, and other noxious substances in the air. Twenty-five percent of disaster recovery workers at “Ground Zero” complain of serious respiratory problems.Doing Post-Event Processing and Debriefing (EPD) with victims of disasters, this author focuses on helping victims to normalize their daily routines, and formulate and develop effective coping strategies. Contemporary ideas on early debriefing will be discussed later in this article when the fifth phase of the recovery process is presented. Many victims and family members seen complained of shock, fear, grief, anger, empty, and of having lost a sense of innocence. But they spoke, above all else, of not being able to relax-of being hypervigilant, hyperalert, distrustful. Many stated that the inner pieces no longer fit, as they realized that their lifelong held assumptions about the world as safe, stable, predictable, rational, and fair were shattered. Now, they were forced to re-evaluate their own prior beliefs about safety, predictability, and universal goodness. Meeting victims’ immediate practical needs for solving resources problems is also very useful during this phase.The preferred approach to helping victims during the EAC phase is to offer vital trauma information, and teach the necessity for seeking and receiving sustenance from naturally-occurring support networks-family members, friends, member of the community, the clergy, and others. These networks offer potentially healing presences of people who are available for empathy, sympathy, and emotional nurturing. Immersion in social networks is more than mere support in the ordinary sense: The network ensures human connections that help victims process their trauma on the emotional level, effecting changes on the neurobiological level as well. Also, these connecting networks help overturn victims’ deleterious avoidance tendency to isolate and avoid interactions with people and the general post-trauma environment. Informal groups consisting of victims, family members, and other victims of previous trauma in sync with the new victims, are helpful in finding emotional resolution and integration.Victims are also encouraged to continually strive to discover new strategies for relaxation. But the relaxing being recommended here is not just sitting down in a quiet place, watching television, and sipping a favorite beverage. Since stress-related hyperarousal is a culprit in the evolution of normal stress into PTSD (a serious health problem with the potential for disrupting the individual’s entire lifeline), relaxing (or stress management) takes on a very special and pressing significance. As a relatively severe and noteworthy stress response, hyperarousal is associated with panic attacks, emotional dyscontrol and lability, increased heart rate and respiration, sleep problems, being easily startled, irritability, agitation, cardiovascular reactivity, and the subjective sense of internally “falling apart.” Hyperarousal during this early phase predicts PTSD (Brende & Parson, 1985; Bryant et al., 2001; Shalev, 1998), as does dissociation-feeling dazed, stunned, numbed to the reality of the calamity (Brende, 1998), and disconnected from parts of self. If severe distress from these symptoms persists after three months and interfere with the individual’s daily functioning, professional intervention that include traumatherapy and drug therapy may be necessary.This writer convinced many New York City victims to turn off the television, and to shut out trauma-related stimuli as a daily practice for days or weeks. Additionally, some persons did daily physical exercise to relieve stress, while inducing feelings of calm and sense of control over their minds and bodies. Some found a re-commitment to faith and religious practice to be a calming and reassuring presence, reducing hyperarousal and associated problems.Victims are encouraged to go easy, and allow self to heal at its own pace. Patience will be required here. They’re also implored talk frequently about the emotional climate that now dominate their internal lives. For some, talking will be difficult; but there is a way out for them. Because of the convincing evidence from research and clinical observation, this author encourages victims to engage in surface journaling (recording their fears, anxieties, catastrophic expectations, sadness, and grief, as well as feelings of elation, triumph, and positive vistas and insights on paper). This form of mental exercise is an excellent counterpart to highly recommend physical exercise, good, nutritious eating, stretching, walking, adequate sleep, and maintenance of normal actional routine, dancing, art, and laughter.The EAC phase is key to preventing PTSD, and it is during this phase that primary care screening for stress symptoms and PTSD is most emphatically recommended. Clinical experience and scientific studies strongly recommend the use of brief screening devices to gather key information to be used to identify persons at risk for PTSD, and especially chronic forms of the disorder. Identification of risk factors is imperative during this time, among these may be added poverty and lack of essential resources, homelessness, and chronic medical illness.Victims with a history of trauma, mental disorder, family psychiatric history, impoverished social supports and resources, need to be identified early to receive appropriate interventions, even during the EAC phase. In such cases it would be prudent for professional helpers to obtain informed consent from victims (Gist and Woodall, 2000). Specific instruments that assess PTSD, severe bereavement reaction, depression, substance abuse, eating disorder, panic disorders, psychotic symptoms, and other mental disorders.Intense psychological debriefing in which painful memories are resurrected and revivified, is to be avoided during this phase. Any memory-activating procedure may prove to paradoxically prove harmful, failing to produce the expected positive therapeutic outcomes. This writer does not see victim assistance during this phase to be “treatment” or “psychotherapy” in the ordinary sense.Phase 2-Stress Response Control (SRC)While the EAC phase represents the time when the victim was caught off guard by an onslaught of overwhelming stimuli, the first response control phase is when the victim’s mind and body attempts to take back control. This phase begins immediately after the traumatic event, and extends to the eighth and twelfth weeks. The first psychobiological event in attempting to heal from disaster trauma is the mind’s own imposition of control over being “swept away” by torrents of powerful emotions, disorganization, and sense of helplessness. The victim attempts to transform disorganizing shock, mental confusion, and hyperarousal of the Emergency Phase into a new mental state that offers control-in the form of emotional numbing, denial, and avoidance of the untoward effects of the disaster upon one’s life. Thus, in this phase the survivor protects self by burying the traumatic experience in the mind and body (Brende & Parson, 1985).Numbing and disbelief yield relief from the emotional shock and internal torture of the trauma, but with this relief the victim’s mind evolves to an awareness of being alive and safe, and the associated self-responsibility. Then, realization and the need for action become preeminent. Providing the stress responses are within tolerable limits for the victim, it is recommended that stress management procedures are used frequently. The procedures include includes one hour a day stretching, breathing, meditation, progressive relaxation, and group support. These awareness and concentration excercies can help quiet down the mind and body.Phase 3-Reenactment and Mastery (RAM)Whereas Phase 2 was characterized by a false sense of all-powerfulness in which numbing and an “above-it-all” denial were key factors, this phase is marked by a false sense of all-powerlessness in which reenactments of the past prove internally overwhelming. During this phase the victim experiences painful memories and a sea of turgid emotions. He or she now is caught up in the realization that life has been permanently altered, and that pre-trauma life is gone forever. RAM is characterized by intrusive thoughts that alternate with numbing and denial. This biphasic processing of trauma is motivated by the mind’s search for a means of mastering the painful memories and emotions associated with the disaster. This processing then leads to reappraisal and realization as the trauma is assimilated into the victim’s pretrauma personality. This processing takes into account the meaning of coming close to death yet remaining alive as recovery and reconstruction moves ahead (Brende, 1998; Brende & Parson, 1998; McFarlane & Raphael, 1984).The alternating between intrusion and numbing is motivated by a biological, subconscious need to master the trauma, and thereby ameliorate the extremes of deep numbing (so closely associated with death and vulnerability in the mind) and disquieting intrusion (so closely associated with being out of control, leading to dissolution of the self). Complicating life in this phase is the accompanying awareness of contending with injuries, job and career setbacks, altered relationships at home and work, repairing property, relocation, role changes, and a lost of past innocence about self and world. Sleep disturbance is prevalent during this phase.Phase 4-Cynicism and Reflective-Transition (CRT)The realization of loss, the general alteration of one’s life, and failure of the authorities to warn and protect against the disaster, may lead to hostility and cynicism in victims. These issues often begin early in the stress recovery process, and persist for several months often with intensity. Victims who had tried to be patient and adapt to a new post-trauma reality may now be feeling rebellious, irritable, cynical, as they complain and show increased irritability, intolerance, and distrust of people. They often feel mistreated by powerful people who neglect, are dishonest, and show little caring for the victim’s plight. In the absence of humor, and their distrust of people who were spared the trauma, as well as the neglecting authorities, victims may be prone to angry or even violent outbursts in close relationships. Making things worse, some victims also suffer physical symptoms, may complain of headaches, nausea, vomiting, muscle aches, chest pain, restlessness, sweating, general fatigue (Brende, 1998; Brende & Parson, 1985; Dahl, 1989), and the complication of alcohol or drug abuse. Some will suffer with significant physical symptoms, pain, and disability, deepening anger and cynicism.During this phase, additionally, there is room for a positive transition based upon reflection and development of a larger personal perspective on the trauma. Here, the victim thinks more about the future than about the past (Brende & Parson, 1985). Though earlier in this phase victims appear to be more affected by loss than they are by gain and advantage, their focus now is on gratitude, and awareness of personal growth, and the future of possibilities (at being alive and surviving one’s own mortality). The last phase, as conceptualized here, is ushered in either when the victim transitions to developing a positive perspective on the trauma or maintains traumatic mental and behavioral patterns.Phase 5-Trauma Stress Renewal Vs. Onset Of Stress Disorder (TR/SD).Most victims exposed to mild to moderate psychological trauma will, as noted before, recover within weeks or months. However, for those victims whose stress responses get worse rather than remit over time, the more likely it is that they will require interventions that go beyond ordinarily psychological debriefing. Generally, after four to six weeks victims will either resolve post-traumatic stress symptoms or find their symptoms are getting worse, becoming ingrained in their minds and bodies. The symptoms of flashbacks, hyperarousal, nightmares, numbing and avoidance, guilt, anger, resentment, irritability, depression, panic attacks, sleep disturbance, and depression may deteriorate into a chronic PTSD and PTSD comorbidities (multiple mental disorders). According to research studies, victims’ gender, age, degree and duration of exposure, prior trauma, negative recovery environment, and the absence of supportive social networks or relationships determine the PTSD outcome.Preventing normal acute stress disorder from evolving into full-blown PTSD should be done whenever possible. If the goal of intervention is reduction of hyperarousal, catastrophic cognitive tendency, and helplessness then research has demonstrated that the most effective treatment for PTSD is cognitive-behavioral therapy with an exposure-based organization (Foa, Hearst-Ikeda & Perry, 1995; Bryant, Harvey, Dang, Sackville, and Basten, 1998; Smyth, 1999). What is still not very clear is whether reduction or management of distress is the best outcome over time for victims. In situations where the disaster trauma was caused by human design, therapy may also need to go beyond symptom relief to dealing with internalized attitudes about dreadful people.ReferencesAmerican Psychiatric Association (1994). Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.Washington, DC: American Psychiatric Association. Ballou, C. (2001, October 23). Does WTC Attack Have a Unique Effect on Veterans? Caribbean Life- Brooklyn and Staten Island, p. 22. Brende, J. O. (1998). Coping with Floods: Assessment, Intervention, and Recovery Processes for Survivors and Helpers. Journal of Contemporary Psychotherapy, 28, 107-140. Brende, J. O. & Parson, E. R. (1985). Vietnam Veteran: The Road to Recovery. New York: Plenum Publishing Corporation. Bryant, R. & Harvey, A. (2000). Acute Stress Disorder: A Handbook of Theory, Assessment, and Treatment.Washington, DC: American Psychological Association. Bryant, R. & Harvey, A. (1997). Acute Stress Disorder: A Critical Review of Diagnostic Issues. Clinical Psychology Review, 17, 757-773. Bryant, R. & Sackville, T., Dang, S., Moulds, M. Guthrie, R. (1999, November). Treating Acute Stress Disorder: An Evaluation of Cognitive Behavior Therapy and Supportive Counseling Techniques. American Journal of Psychiatry, 156, 1780-1786. Foa, E., Hearst-Ikeda, D., & Perry, K. (1995). Evaluation of a Brief Cognitve-Behavioral Program for the Prevention of Chronic of Chronic PTSD in Recent Assault Victims. Journal of Consulting And Clinical Psychology, 63, 948-955. Nervous and Mental Disease, 187, 661-672. Lonigan, C., Anthony, J. Shannon, M. (1998). Diagnostic efficacy of post-traumatic symptoms in children exposed to disaster. Journal of Clinical Child Psychology, 27, 255-267. McDermott, B., & Palmer, L. (1999). Post-disaster service provision following proactive identification of children with emotional distress and depression. Australian and New Zealand Journal of Psychiatry, 33, 855-863. McFarlane, A. & Hua, C. (1993). Study of a major disaster in the People’s Republic of China: The Yunnan earthquake. In J. P. Wilson & B. Raphael (Eds.), International Handbook of Traumatic Stress Syndromes (pp. 493-498). New York: Plenum Press. National Oceanic and Atmospheric Administration, 2002). Billion Dollar U.S. Weather Disasters, 1980- 2001. National Center Climatic Data Center (NCDC), January 1, 2002. Parson, E. R. (1994). Post-Traumatic Stress Disorder: Its Biopsychobehavioral Aspects and Management. In B. Wolman & G. Stricker (Eds). Anxiety and Related Disorders: A Handbook (pp. 226-285). New York: Wiley. Parson, E. R. (1995a). Adaptational Coping with Mass Traumatic Terror. Journal of Contemporary Psychotherapy. Parson, E. R. (1995b). Adaptational Coping with Mass Traumatic Terror. Journal of Contemporary Psychotherapy. Raphael, B. (2000). Disaster Mental Health Response Handbook. Shalev, A., Sahar, T., Freedman, S., Peri, T., Click, N., Brandes, D., Orr, S., & Pitman, R. (1998). Predicting PTSD in Trauma Survivors: Prospective Evaluation of Self-Report and Clinician- Administered Instruments. British Journal of Psychiatry, 170, 558-564. Smyth, L. (1999). Cognitive-Behavioral Treatment of Anxiety Disorders. Havre De Grace, MD: RTR Publishing Company. Erwin R. Parson, (1943-2006) Ph.D., A.B.P.P. was a Diplomate in Psychology, a Master Clinician and Trauma Treatment Technology Developer for over 20 years. Having worked in the area of administration of trauma programs, Dr. Parson also worked in the direct treatment of trauma adult and child victims. He was the author of dozens of articles and book chapters in the area of trauma, ethnicity, and healing.  PDF [221KB] PDF [221KB] |
